Joy L. Moeller, R.D.H., B.S.
Joy L. Moeller, R.D.H., B.S.
Volume 30 Issue 4 October 2012
Editorial:
It is said that timing is everything. You may have heard of orofacial myofunctional therapy (OMT) popping up here and there in the U.S. over the past few decades. In 1978, I ventured into this field eager to learn more about the mouth exercises my son had benefited from as a patient with TMD. I studied the therapy rigorously, attending several courses with Dan Garliner and others who, at the time, were leaders in this field. While U.S. institutional interest in the field over the past few decades has waxed and waned for various reasons, early OMT specialists have continued to practice, train others, and steadily build awareness through clinical success.
You may have seen an increase in discussion of the field in the last year or two. A quick search using Google will show a seven-fold rise in “myofunctional therapy” searches from 2011 to 2012. Why is this interdisciplinary field, which has shown promise of success yet not quite taken off as a profession, suddenly come into greater prominence? With new research from Brazil and OMTs proven efficacy in treating TMD1 and OSA,2 the field is poised to explode like never before.
Around the time I began, a few Brazilian speech pathologists, visionaries like Drs. Irene Queiroz Marchesan and Esther Mandelbaum Goncalves Bianchini, studied these same courses. Bringing this knowledge home, they enhanced and implemented OMT into academic environments and successfully fought for national recognition.
Three factors combined to make the profession take off: strategic leadership, the healthcare marketplace, and a vigorous research environment. These ingredients, under the banner of “Ordem e Progresso” have resulted in Brazil being the first and only country to have federal licensure in the field. With over 20 universities engaged in research, Brazil has effectively thrust OMT into the spotlight. We now have the evidence-based research we need to support the benefits of OMT as it relates to TMD and OSA. Just this year in June at the Brazilian Orofacial Myology Association Congress, hundreds of new OMT research posters were presented, and this November in Brazil at the Brazilian Speech Society (SBFa) Congress, there will be hundreds more.
OMT, also known as neuro-muscular re-education of the oral facial muscles, is a modality that promotes the stability of the stomatognathic system. Studies have been done for centuries to understand the relationship of form and function.3 When the tongue is resting against the hard palate (thus maintaining the proper oral volume) it enhances and/or creates stability for the TMJs. If the tongue is habitually resting down and forward in the mandible, as may happen with a lack of patency of airways and/or excessive use of bottles, pacifiers, digit sucking4 or a restricted frenum,5 normal form and function may be disrupted.6
While a primary function of the tongue is to protect the airway, improper oral resting posture of the tongue will have a negative influence on the development of the oral cavity. Add that to the modern diet of processed foods (soft foods may lead to low muscle tone by diminishing the frequency and intensity of mastication7), a smaller oral volume may not support proper upper airways, the stability of the TMJs, or the development of optimal dental arches.8
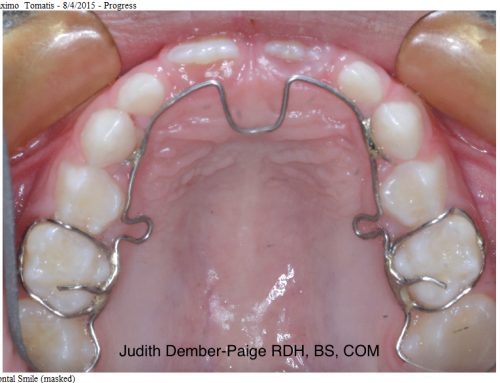
OMT specialists are trained to promote functional posture9 (in absence of mechanical obstruction) with behavior modification. The goals for the patient are to become aware of, and eliminate, noxious habits and achieve nasal breathing, lip seal, and proper mastication. OMT specialists also promote patient compliance in the proper care and use of oral appliances that treat TMD and OSA, as well as minimize muscular discomfort due to the use of those appliances.
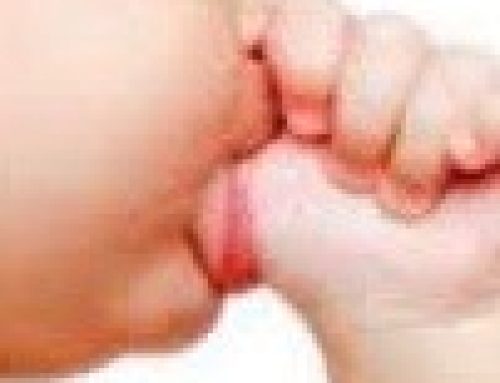
Contributing to the creation of orofacial myofunctional disorders (OMDs) are restricted lingual frena.5 It used to be that a baby’s tongue was checked immediately upon birth to make sure the baby could breastfeed easily. Possibly due to the proliferation and universal acceptance of bottle-feeding, a restricted lingual frenum is not only overlooked by healthcare professionals, but its detrimental effects are not fully understood.
Tight lingual frena have a critical impact on normal function and the development of the orofacial complex. The restricted frenum not only may affect the oral resting posture of the tongue, but it also disrupts the tongue muscles, both intrinsic and extrinsic, of their normal functions. If the frenum is restricted, the genioglossus muscle may not function normally and may impact the airway patency and contribute to sleep disordered breathing.11 Furthermore, the attachments of the tongue to the mandible may restrict forward growth and development. Lingual frenectomies are essential if the tongue is restricted for a full range of mobility. And even more essential is the follow-up with an OMT specialist so that the patient who has just undergone a lingual frenectomy may be assured success. The OMT specialist will work with the patient to re-pattern the muscles, ensure full range of motion of the tongue, and make sure the tissues do not re-attach after surgery.
It is ideal to release the restricted frenum as early as possible-meaning at birth-because the tongue will achieve optimal function through the activity of breastfeeding. Breastfeeding promotes tongue-palatal contact and requires the back of the tongue to activate by making a suction seal. These actions promote optimal muscle function of the entire orofacial complex.
Much more research is needed in this field to fully embrace how we may all benefit from OMT, practitioners and the public alike. Not a week goes by where a patient doesn’t say, “How come I didn’t know about this sooner? It could have saved me so many years of pain.” It breaks my heart that more people don’t know about OMT. I dream of a day when the United States will “catch up” to Brazil and implement this field into academic arenas, where research is promoted, where studies open doors to more physicians, more dentists and more patients who need this treatment. We are poised to rapidly advance this field. In just the past year, several leading professional healthcare organizations have sought speakers on OMT, and several of our leading universities have begun discussions about starting research. If timing is everything, I feel like I’m finally arriving, but it took me 30 years to get here. Our patients are asking for help. Don’t we owe it to them to offer this adjunctive treatment?
Joy L. Moeller, R.D.H., B.S.
Orofacial Myofunctional Therapist
Pacific Palisades, California
www.myofunctional-therapy.com
joyleamoeller@aol.com
www.facebook.com/oralmyology
References
1. de Felicio CM , de Oliveira Melchior M, Antonio M, da Silva MR: Effects of orofacial myofunctional therapy on temporomandibular disorders.
J Craniomandib Pract 2010; 28:249-259.
2. Guimaraes K, et al.: Effects of oropharangeal exercises on patients with moderate sleep apnea. Am J Respir Crit Care Med 2009; 179:962-966.
3. Levrini A, Favero L: The masters of functional orthodontics. Quintessence, 2003.
4. Romero C. et al.: Breastfeeding and non-nutritive sucking patterns related to the prevalence of anterior open bite in primary dentition. J Appl Oral Sci 2011; 19:2:161-168
5. Northcutt M: Overview the lingual frenum. JCO 2009; 18:557-565.
6. Rogers AP: Exercises for the development of muscles of the face with view to increasing their functional activity. Dental Cosmos LX 1918; 59:857-876.
7. Rapley G, Murkett T: Baby-led weaning. England: Vermilion, 2008.
8. Price W, Pottenger F: Nutrition and physical degeneration: a comparison of primitive and modern diets and their effects. New York: P.B. Hoeber, 1939.
9. Okuro R., et al.: Mouth breathing and forward head postural effects on respiratory biomechanics and exercise capacity in children. J Bras Pneumol 2011; 37: 4:471-479.
10. Hsu H-Y, Yamaguchi K: Decreased chewing activity during mouth breathing. J Oral Rehabil 2012; 39(8):559-567.
11. Mathur R, et al.: Effect of breathing, pressure and posture on palatoglossal and genioglossal tone. Clin Sci (Lond), 1995; 89:441-445.
© 2009-2013: The Journal of Craniomandibular Practice. Site by Medium